Heart Disease: Your Guide to Symptoms, Causes, and How to Fortify Your Defenses
Let’s talk about your heart. Not the one that races when you see your crush or breaks during a sad movie, but the magnificent, fist-sized engine in your chest that’s been working tirelessly for you since before you were born. It beats roughly 100,000 times a day, pumping life through your veins. But what happens when this incredible machine starts to sputter? Heart disease isn’t just a headline or something that happens to “other people.” It’s the leading cause of death globally, but here’s the crucial part: it’s also largely preventable.
I learned this the hard way. My wake-up call wasn’t a dramatic clutch of the chest. It was a routine physical in my late 30s. I felt fine—a little tired, maybe, but I chalked that up to work and life. My doctor, however, saw a different story. My blood pressure was flirting with the danger zone, and my LDL cholesterol (the “bad” kind) was throwing a party in my bloodstream. My family history, which I’d blissfully ignored, suddenly felt like a looming shadow. That day, the term “heart disease” shifted from an abstract concept to a very personal, very avoidable future. This article is the one I wish I’d read back then. It’s a blend of deep research, expert guidance, and a personal journey to help you understand your heart and, more importantly, protect it.
What is Heart Disease? More Than Just a “Heart Attack”
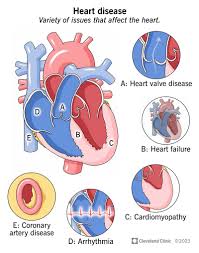
When we say “heart disease,” we’re usually talking about cardiovascular disease (CVD), an umbrella term for a host of conditions that affect your heart and blood vessels. It’s not a single ailment but a category, and understanding its forms is the first step to fighting it.
The Most Common Culprit: Coronary Artery Disease (CAD)
Think of your coronary arteries as the vital supply lines delivering oxygen-rich blood to your heart muscle itself. Coronary artery disease (CAD) is what happens when these critical pipelines get clogged.
How CAD Develops: The Silent Siege
The process begins with atherosclerosis, a fancy word for a simple, dangerous process: the buildup of fatty deposits called plaque inside your artery walls. Imagine it like rust and gunk slowly accumulating in an old pipe. Over years, even decades, this plaque narrows the arteries, reducing blood flow to the heart. This can lead to chest pain (angina) or, if a plaque ruptures and causes a complete blockage, a heart attack.
Other Key Players in Heart Disease
While CAD is the star of the show, the supporting cast can also cause major trouble.
- Heart Failure: This doesn’t mean the heart stops. It means it’s weakened and can’t pump blood as efficiently as it should, leading to fatigue, shortness of breath, and fluid buildup.
- Arrhythmia: This is an irregular heartbeat—too fast, too slow, or just erratic. It can feel like a fluttering or a racing heart and can be dangerous if it disrupts blood flow.
- Heart Valve Problems: Your heart has valves that act as doors to ensure blood flows in one direction. If these doors are damaged, they can leak (regurgitation) or become narrow (stenosis), straining the heart.
Listening to the Whispers: Recognizing the Symptoms of Heart Disease
Your body is an excellent communicator; the problem is we’re often terrible listeners. Heart disease symptoms can be dramatic, but more often, they are subtle whispers we easily dismiss as something else.
Symptoms of Coronary Artery Disease
The classic sign is angina: a discomfort, pressure, squeezing, or pain in the chest. But it’s sneaky. It can also manifest as:
- Pain in the neck, jaw, throat, upper abdomen, or back.
- Shortness of breath during routine activity.
- Crushing fatigue that feels different from normal tiredness.
When It’s an Emergency: Heart Attack Symptoms
A heart attack is a “code red.” Knowing these signs can save your life or someone else’s. They include:
- Chest pain or discomfort that doesn’t go away (pressure, squeezing, fullness).
- Pain radiating to one or both arms, the back, neck, jaw, or stomach.
- Shortness of breath, with or without chest discomfort.
- A cold sweat, nausea, lightheadedness, or a sense of impending doom.
Important Note: Symptoms can vary greatly between men and women. Women are more likely to experience shortness of breath, nausea/vomiting, and back or jaw pain without the classic chest pressure.
Symptoms of Other Heart Conditions
- Arrhythmia: Feelings of a fluttering, racing, or slow heartbeat (palpitations), chest pain, dizziness, or fainting.
- Heart Failure: Shortness of breath, fatigue, swelling in the legs, ankles, and feet due to fluid buildup.
- Valve Disease: Shortness of breath, fatigue, irregular heartbeat, swollen feet or ankles, and chest pain.
The Root of the Problem: Unpacking the Causes of Heart Disease
So, how does this silent siege begin? It’s rarely one thing. It’s a perfect storm of factors, some within your control and some not.
The Non-Modifiable Risk Factors (The Cards You’re Dealt)
These are the factors you can’t change, but knowing them should make you more vigilant, not less.
- Age: Simply put, the older you get, the higher your risk.
- Sex: Generally, men are at greater risk. However, a woman’s risk increases after menopause.
- Family History: If a close relative had early heart disease, your risk is higher. This was my red flag.
- Race: Certain ethnicities, including African Americans, have a higher predisposition.
The Modifiable Risk Factors (The Cards You Can Play)
This is where your power lies. These are the causes you can directly influence through lifestyle choices.
- Unhealthy Diet: A diet high in saturated fats, trans fats, salt, and sugar is public enemy number one for your arteries.
- Physical Inactivity: A sedentary lifestyle is a direct ticket to weight gain, high blood pressure, and poor heart health.
- Smoking: This is arguably the single worst thing you can do for your heart. It damages the lining of your arteries, drastically accelerating plaque buildup.
- Excessive Alcohol Consumption: Heavy drinking can raise your blood pressure and contribute to heart failure.
- Chronic Stress: Unmanaged stress can damage your arteries and worsen other risk factors.
The Medical Conditions That Pave the Way
Certain health conditions act as powerful accelerants for heart disease. Managing these is a direct form of prevention.
- High Blood Pressure (Hypertension): This is the constant force of blood pounding against your artery walls, eventually causing damage that invites plaque.
- High Cholesterol: Specifically, high levels of LDL cholesterol lead directly to plaque formation.
- Diabetes: High blood sugar levels can damage blood vessels and the nerves that control your heart.
- Obesity: Excess weight, especially around the abdomen, forces your heart to work harder and is linked to other risk factors.
Your Blueprint for a Healthy Heart: How to Prevent Heart Disease
Now for the good news—the empowering part. Preventing heart disease is about building a fortress around your heart, one healthy habit at a time. It’s not about deprivation; it’s about celebration of what your body can do when you fuel and move it properly.
Fueling Your Engine: The Heart-Healthy Diet
Forget fad diets. This is about a sustainable, delicious way of eating.
- Embrace Plants: Fill half your plate with a rainbow of fruits and vegetables.
- Choose Whole Grains: Swap white bread and pasta for whole-wheat, oats, quinoa, and brown rice.
- Pick Healthy Fats: Avocados, nuts, seeds, and olive oil are your friends.
- Go Lean on Protein: Opt for fish (especially fatty fish like salmon twice a week), skinless poultry, beans, and lentils.
- Drastically Reduce: Sodium (salt), processed foods, sugary drinks, and red meat.
Getting Moving: Exercise as Medicine
You don’t need to train for a marathon. Consistency is key.
- Aim for 150 minutes of moderate-intensity aerobic exercise (brisk walking, cycling, swimming) per week. That’s just 30 minutes, 5 days a week.
- Add strength training at least two days a week. More muscle helps manage weight and blood sugar.
- The best exercise is the one you’ll actually do. Find something you enjoy!
Kicking the Habits: Smoking and Alcohol
- Quit Smoking. Full stop. It’s the most significant positive change you can make for your heart.
- Limit Alcohol. If you drink, do so in moderation. That’s up to one drink a day for women and two for men.
The Mind-Heart Connection: Managing Stress
Chronic stress is a silent killer. Find your release valve:
- Practice mindfulness, meditation, or deep breathing.
- Connect with friends and family.
- Pursue hobbies that bring you joy.
- Ensure you’re getting enough quality sleep (7-9 hours per night).
Partnering with Your Doctor: The Power of Knowledge
You can’t manage what you don’t measure.
- Know Your Numbers: Get regular check-ups to monitor your blood pressure, cholesterol, and blood sugar levels.
- Follow Medical Advice: If you have hypertension, high cholesterol, or diabetes, diligently take prescribed medications. They are vital tools in your prevention toolkit.
A Side-by-Side Look: Lifestyle Choices & Their Impact
| Your Choice | The Heart-Harming Path | The Heart-Healthy Path |
|---|---|---|
| Diet | Processed foods, red meat, sugary snacks, high salt. | Colorful plants, whole grains, lean protein, healthy fats. |
| Activity | Sedentary lifestyle, sitting most of the day. | Daily walks, taking the stairs, regular workouts you enjoy. |
| Stress Mgmt | Ignoring stress, no outlets, poor sleep. | Meditation, hobbies, social connection, 7-9 hours of sleep. |
| Doctor Visits | Avoiding check-ups, not knowing your numbers. | Regular screenings, managing conditions, taking meds as prescribed. |
People Also Ask (PAA) About Heart Disease
What are the early signs of heart disease?
Early signs are often subtle and can include unusual fatigue, slight shortness of breath during normal activities, minor chest discomfort (angina), or heart palpitations. Listening to these small whispers from your body is key to early detection.
Can heart disease be reversed?
While you can’t entirely “reverse” it, you can absolutely halt its progression and significantly reduce its impact through aggressive lifestyle changes and medication. This process, called disease regression, can dramatically improve your health and quality of life.
What is the best exercise for your heart?
Aerobic exercises that get your heart pumping are best. This includes brisk walking, jogging, swimming, and cycling. The “best” exercise is ultimately any activity you enjoy enough to do consistently, 30 minutes a day most days of the week.
How can I test my heart health at home?
While you can’t run a full diagnostic at home, you can monitor key indicators. Use a home blood pressure monitor to track your BP, track your resting heart rate (lower is generally better), and pay attention to your body’s signals during activity, like how quickly you become short of breath.
What is the #1 food for your heart?
There isn’t one single magic food. The best approach is a dietary pattern. However, if we had to pick a superstar, it would be fatty fish like salmon, mackerel, or sardines, which are rich in omega-3 fatty acids that powerfully fight inflammation and protect blood vessels.
Frequently Asked Questions (FAQ)
Q: Can young people get heart disease?
A: Absolutely. While risk increases with age, the process of atherosclerosis can begin in childhood and adolescence due to poor diet and inactivity. Heart attacks in people in their 20s and 30s, while less common, do happen. It’s never too early to adopt heart-healthy habits.
Q: How does sleep affect heart health?
A: Profoundly. Poor sleep (consistently less than 7 hours) is linked to higher blood pressure, weight gain, and inflammation. Conditions like sleep apnea, which disrupts breathing during sleep, are a major risk factor for hypertension and heart disease.
Q: Are all fats bad for the heart?
A: This is a huge misconception. Unsaturated fats (found in olive oil, nuts, avocados, and fish) are incredibly beneficial for heart health. The fats to avoid are trans fats (often in processed foods) and to limit saturated fats (found in red meat and full-fat dairy).
Q: Is wine good for your heart?
A: The evidence is mixed and controversial. Some studies suggest antioxidants in red wine may offer benefits, but these are likely outweighed by the risks of alcohol consumption, including increased blood pressure and calorie intake. You should not start drinking for heart benefits. The proven benefits of diet and exercise are far more significant.
Q: How often should I get my cholesterol checked?
A: Adults aged 20 and older should have their cholesterol checked every 4 to 6 years if they are at low risk. If you have risk factors like family history, high blood pressure, or are overweight, your doctor will likely recommend more frequent testing, such as annually.
Protecting your heart is the ultimate long game. It’s the sum of a thousand small choices—the apple over the doughnut, the walk around the block, the deep breath during a stressful moment. It’s not about perfection; it’s about progression. My own journey started with that scary doctor’s visit. I began with small swaps—Greek yogurt instead of sour cream, walking meetings instead of sitting ones. I learned to read nutrition labels like a detective. It was a slow process, but at my next check-up, seeing my numbers move in the right direction was one of the most rewarding feelings of my life. Your heart has been there for you every second of your life. Isn’t it time you returned the favor? Start today.